It was first noticed that the rate of erythrocyte sedimentation changed owing to illness in the 1700s. The use of this attribute as a measure of inflammatory activity due to underlying disease was formalized into a test in the early 1900s and what has become known as the Westergren test has again recently been proposed to be the reference method for measuring erythrocyte sedimentation rate, which is still a commonly used hematology test today. This article allows you to understand why it is used, how the results are affected by physiological factors and how to perform it to obtain useful and reliable results.
Using erythrocyte sedimentation rate measurement to indicate inflammation
Explaining erythrocyte sedimentation rate measurement
The erythrocyte sedimentation rate (ESR) is a general condition indicator and serves as a guide to determine diagnosis and treatment follow-up of different autoimmune diseases, acute and chronic infections and tumors. ESR is the speed at which erythrocytes settle in a tube and provides medical practitioners with valuable information for the diagnosis of their patients. Normal-sized erythrocytes are negatively charged and repel each other, which limits their sedimentation rate. Erythrocytes that form clumps fall faster than small ones, so factors that increase aggregation will increase sedimentation. This increased sedimentation indicates health problems, resulting in a need for additional tests.
Applications of ESR measurement
There’s a long list of conditions for which ESR can be used to assist in making a correct diagnosis or managing the care of a patient: autoimmune diseases such as rheumatoid arthritis, temporal arteritis and polymyalgia rheumatica are well known examples, as is multiple myeloma. When the presence of inflammation is suspected, ESR is a simple and cost-effective way of confirming this. Moreover, for patients with a known condition, the ESR test can provide useful information into the overall effectiveness of their treatment.
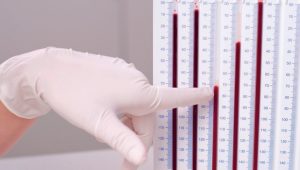
The Westergren method
The discovery of the ESR dates back to 1794, but in the 1920s, pathologist Robert Fåhraeus and Alf Westergren developed ESR measurement as we know it. To this day, the so-called Westergren method is recognized as the gold standard, among others by the Clinical and Laboratory Standards Institute (CLSI). In 2017, the International Council for Standardization in Hematology (ICSH) reconfirmed the Westergren method as the reference method for ESR measurement. The Westergren method owes its popularity to the fact that it’s a simple and inexpensive first-line test, providing valuable information to GPs in the investigation of inflammation after only 60 (or even 30) minutes.
Critical factors of a reliable ESR test
Although the Westergren method may be the gold standard, many factors can meddle with its reliability. Therefore, always keep in mind the following requirements:
- non-hemolysed blood anti-coagulated with EDTA at collection;
- blood sample is thoroughly mixed and diluted 4 :|1 using a sodium citrate solution;
- the tube is held in vertical position at a constant temperature (±1 °C) between 18 °C and 25 °C in an area free from vibrations, drafts and direct sunlight; and
- results are interpreted after at least 30
Can we speed up ESR measurement?
In the original Westergren method, the ESR is read after 60 minutes. You can imagine this puts practical limitations on the workflow in clinical laboratories. A laboratory investigation, however, showed that 30-minute ESR readings correlate highly with the corresponding 60-minute ESR readings, which is why today most laboratories perform 30-minute ESR readings and then extrapolate them to derive the 60-minute ESR result. There are Westergren alternatives that claim to measure ESR after only 20|seconds, but as it takes at least 10 minutes before sedimentation starts at a constant rate, these tests risk leading to a number of false negatives.
Why speeding up ESR measurement is not a good idea
The Westergren method and faster alternatives
As mentioned above, the 30-minute version of the Westergren test has become the standard in most hospitals and laboratories. However, even though 30 minutes can be regarded as a short time frame, some companies have worked on Westergren alternatives that can be read after mere minutes or even seconds. A major step forward, or so it seems.
What’s the deal with fast ESR measurement methods?
There are several conditions that ESR methods should comply with in order for them to be reliable. For example, test tubes must be held in vertical position, and the blood must be thoroughly mixed and diluted. Still the most important condition of all doesn’t revolve around equipment; it revolves around time. It takes approximately 10 minutes before red blood cell sedimentation starts at a constant rate. This means that ESR readings after 20 seconds do not actually measure sedimentation but calculate a mathematically derived ESR. This, in turn, leads to ESR readings that don’t correlate with the Westergren standard, leading to a number of false negatives. So, in their attempt to speed up the diagnosis of patients, laboratories that use Westergren alternatives risk overlooking important signs of disease.
Speed or reliability?
Healthcare and in vitro diagnostics are being improved daily and theories are constantly evolving. This makes it hard to determine which ESR method is the right one to choose. The choice is even harder when you consider that ESR alternatives are comparable to the Westergren method, as long as you treat healthy people under normal circumstances. It’s when people are ill that the results start to deviate. This is why our advice is to always choose a method that adheres closely to the Westergren method [such as automated ESR analysers Starrsed (RR Mechatronics), MixRate and Excyte (ELITech)]. Westergren has always been the method of choice in fundamental studies, meaning that ESR is essentially based on this procedure. Moreover, the Westergren method is recommended by the CLSI and reconfirmed as the gold standard by ICSH, two organizations that inform healthcare professionals on state of the art technologies for in vitro diagnostic testing.
Not everything can be rushed
Moving forward is part of human nature; it’s why we’re always so busy making things better, faster and more comfortable. But in the case of ESR measurement, we simply have to face the fact that not everything can be rushed. We may be able to speed up the way we live, work and travel; we cannot force red blood cells to settle faster than they do. What we can do, is make ESR measurement tests as reliable as possible and have them help us improve diagnostics and save lives.
Physiological and clinical factors that influence ESR values
In the investigation of inflammation, ESR measurement is often the first-line test of choice as it’s simple, inexpensive and – if based on the Westergren method – reliable, reproducible and sensitive. But as is the case with every test, there are physiological and clinical factors that may influence ESR results. In this section, we’ll tell you more about them. However, when reading about factors that influence ESR results, please keep in mind that much, if not all of this information, is based on studies undertaken with the Westergren gold standard ESR method only. This is mainly due to the fact that the Westergren ESR method has been almost universally used to investigate the clinical utility of the test in a range of disease states, with much of this work published in peer reviewed journals. As a result, there’s a deep body of knowledge that describes the impact of disease, the limitations and sources of interference with the Westergren ESR. As the Westergren method for ESR measures a physical process under a defined set of conditions, this expansive body of knowledge cannot simply be ‘transferred’ to estimations of ESR by methods that use centrifugation or optical rheology.
What’s normal in ESR?
Before discussing the factors that influence ESR results, first we should answer the question: what is normal? When patients suffer from a condition that causes inflammation, their erythrocytes form clumps which makes them settle faster than they would in the absence of an inflammatory response. However, ‘faster’ is a relative term, and what’s ‘normal’ changes based on sex and age category (Table 1).
| Sex/age category | Normal ESR (mm/hr) |
| Female <50 years | <20 |
| Male <50 years | <15 |
| Female >50 years | <30 |
| Male >50 years | <20 |
| Children | 0–10 |
Table 1. Normal erythrocyte sedimentation rates (ESR) by age and sex
Physiological and clinical factors that increase ESR
The most obvious explanation for increased ESR is inflammation. During acute phase reactions, macromolecular plasma proteins, particularly fibrinogen, are produced that decrease the negative charges between erythrocytes and thereby encourage the formation of cell clumps. And as cell clumps settle faster, this increases ESR. Inflammation indicates a physical problem, meaning additional tests and follow-up are needed. However, there are other factors that increase ESR but don’t necessarily come with inflammation. For example, ESR values are higher for women than for men and increase progressively with age. Pregnancy also increases ESR, which means you’ll be dealing with ESR results above average. In anemia, the number of red blood cells is reduced, which increases so-called rouleaux formation so that the cells fall faster. This effect is strengthened by the reduced hematocrit, which affects the speed of the upward plasma current. Another factor that increases ESR revolves around high protein concentrations. And in macrocytosis, erythrocytes have a shape with a small surface-to-volume ratio, which leads to a higher sedimentation rate.
Physiological and clinical factors that decrease ESR
Apart from factors that increase ESR, medical practitioners and laboratory scientists should also consider the factors that decrease ESR. This is especially important as decreased ESR results may lead to missed diagnoses, whereas increased ESR results either lead to the right follow-up or false positives. Polycythemia, caused by increased numbers of red blood cells or by a decrease in plasma volume, artificially lowers ESR. Red blood cell abnormalities also affect aggregation, rouleaux formation and therefore sedimentation rate. Another cause of a low ESR is a decrease in plasma proteins, especially of fibrinogen and paraproteins.
The four factors that determine ESR reliability (dos and don’ts)
As with any test, the reliability of ESR measurements stands or falls with proper implementation. When not reliably performed, the non- specific indicator for inflammation may point in the wrong direction, and result in either a false positive or a false negative. This may lead to the initiation of unnecessary investigations or worse: the overlooking of serious problems that actually needed follow-up. In this section, we discuss some do’s and don’ts when performing ESR measurement, to guarantee ESR reliability.
Factor 1: blood collection
Do: make sure you mix and dilute the sample 4:1 using a sodium citrate solution. If you adhere to these practices, you standardize the way you handle the blood samples, and therefore their suitability for ESR. Don’t: leave the sample for too long before testing. We can imagine you’re pretty busy, and that you can’t do everything at the same time. However, when it comes to blood collection for ESR tests, some speed is required. After four hours, the results won’t be as accurate as before, which may negatively impact the reliability of the result. We therefore recommend performing the test within these four hours. If you really can’t make it in time, 24 hours is the max, but only if the sample is stored at 4 °C.
Factor 2: tube handling
Do: hold the tube vertically. A tube that is not held completely vertical can lead to increased sedimentation rates and is one of the technical factors that can affect ESR readings. And as we discussed in the previous paragraph, temperature is a factor too. Therefore, always place the tube in a stable and vertical position and at a constant temperature. Don’t: expose the sample to vibrations, draft and sunlight, as all of these factors can have a strong influence on the final result obtained.
Factor 3: result reading
Do: wait 30|minutes. This is a very important one. Before reading ESR results, you should always wait 30|minutes. There are ESR testing methods that claim to show reliable results within only 20 seconds, but as it takes 10 minutes before sedimentation starts at a constant rate, these tests do not actually measure sedimentation. In fact, they calculate a mathematically derived ESR, leading to a number of false negatives. Don’t: include the buffy coat (which is made up of leukocytes) in the erythrocyte column.
Factor 4: test quality
Do: go with an automated ESR test. They provide you with more reliable results, not least because they can correct hazy results. More- over, automated ESR tests have a higher throughput compared to manual tests and minimize human contact with the tubes, which helps you reduce operations costs and minimize occupational health and safety risks. Don’t: choose an ESR test that deviates from the Westergren standard. This method has always been the method of choice in fundamental studies, meaning that ESR is essentially based on this procedure. ESR tests that deviate from the Westergren will logically provide you with different ESR values, meaning they can lead you in the wrong direction. This is why the Westergren method is recommended by the CLSI and reconfirmed as the gold standard by ICSH.
ESR test as a reliable tool
If you keep these dos and don’ts in mind, you’re well on your way to making the ESR test a reliable tool that’s going to help you diagnose patients fast and error-free.
The author
Peter Murphy MBA(TechMgt), MAACB, BSc, GradDipEd ELITech Group, Braeside, Victoria 3195, Australia E-mail: p.murphy@elitechgroup.com“